In the paper “The impact of obesity‑related raised intracranial pressure in rodents” published in Scientific Reports journal, Westgate and collaborators used the Phoenix MICRON® image-guided OCT system, along with the Phoenix MICRON® Insight software, in the measurement of the retinal anatomical changes caused by intracranial hypertension in obese rats.
The Problem:
Intracranial pressure (ICP) measures the force that the brain and its surrounding tissues produce against the cranial bone. Accumulation of cerebrospinal fluid, brain inflammation, or bleeding — commonly seen in traumatic brain injury, hydrocephalus, or ischemic stroke — increases ICP and causes intracranial hypertension. Occasionally, ICP rises without a clear cause, and it is called idiopathic intracranial hypertension (IIH). Some reports show that people with higher body mass indexes have higher ICP, associating obesity with a high risk of developing IIH. Intracranial hypertension affects the brain and optic nerve causing headaches, cognitive impairment, and swelling of the optic nerve (papilledema) that can progress to vision loss, but the specific anatomical cause that trigger these symptoms is unknown. As a result, there are limited available therapies for management.
The Challenge:
To understand what anatomical changes occur in the obesity-induced intracranial hypertension, Westgate and colleagues developed an animal model for non-traumatic raised ICP whereby they induced obesity in rats.
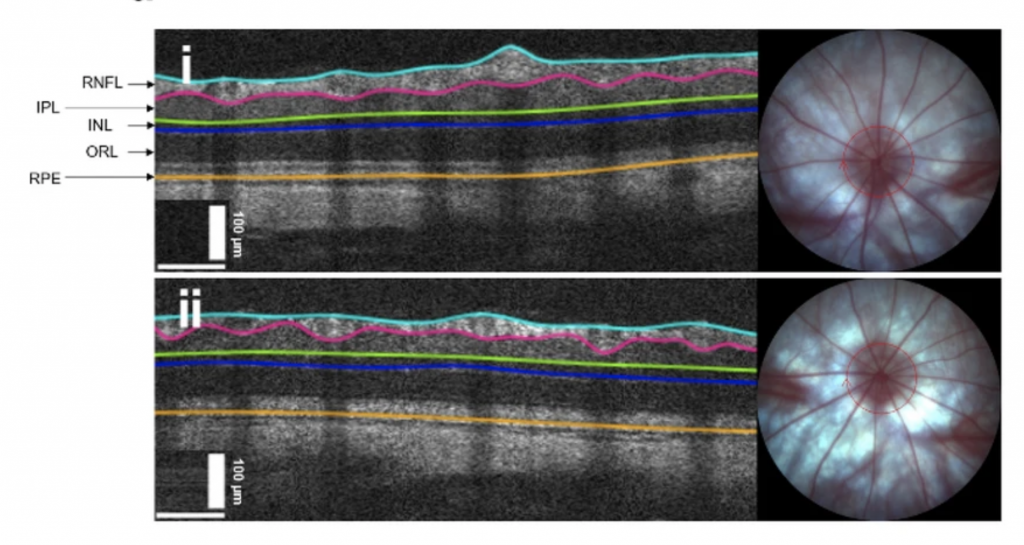
Rats fed a high-fat diet developed obesity by week 15 and showed higher ICP than controls during the first 15 days of monitoring. Interestingly, in obese rats, the researchers found that intracranial pressure positively correlated with their abdominal fat percentage. During the course of the diet, obese rats showed a marked headache behavior demonstrated by their higher cephalic sensitivity to mechanical stimuli and increased expression of pain receptors compared to control rats. To evaluate the retinal anatomy, researchers took optical disc pit (ODP) images and optical coherence tomography (OCT) scans of the retina with the Phoenix MICRON Image-Guided OCT2 system. Additionally, they performed histological observations, measured gene expression, and analysed painful behaviors looking for possible correlations.
The Results:
The obtained images showed normal optic discs in both groups and no signs of papilledema. But analysis of the cross-section retinal images from the Phoenix MICRON OCT with the semi-automatic retinal segmentation software (Phoenix MICRON InSight), showed a thicker nerve fiber layer in obese rats compared to controls. Moreover, they noted that the retinal nerve fiber layer (RNFL) was even thicker in those obese rats that had more abdominal fat, which could explain the positive correlation between the intracranial pressure and the percentage of abdominal fat.
The Phoenix MICRON® Image-Guided OCT2 system has been designed specifically for the demands of in vivo research using mice and rats, delivering extraordinary retinal scan detail.
The OCT2 system includes a live, real-time color fundus display with superimposed scan line to allow precise positioning over retinal features. The system supports 2D capture, and production of 3D volumes, and includes a set of powerful segmentation and visualization tools.
We are delighted to see an example of how the Phoenix MICRON Image-Guided OCT2 in combination with the Phoenix MICRON Insight Software, were valuable tools for studying detailed anatomical retinal changes in this new model of non-traumatic ICP developed by Westgate et al. Their work provides the ability to obtain a specific comparison between health and disease conditions and lays the ground for further study into retinal function and ICP-reducing therapies.
Citation: Westgate, C.S.J., Hagen, S.M., Israelsen, I.M.E. et al. “The impact of obesity-related raised intracranial pressure in rodents.” Sci Rep 12, 9102 (2022). https://doi.org/10.1038/s41598-022-13181-6