 McDaniels et al at the US Army Institute of Surgical Research used the Phoenix anterior chamber OCT to evaluate the safety of an ocular wound chamber after a corneal injury in guinea pigs. The research group developed an ocular wound chamber that encases the eye and allows for controlled delivery of therapeutics and eye lubricant. Using OCT, intraocular pressure measurements, bright field and fluorescein imaging, and histology, they confirmed that the ocular wound chamber is safe for the skin and eye, and does not change wound healing when filled with optical lubricant.
McDaniels et al at the US Army Institute of Surgical Research used the Phoenix anterior chamber OCT to evaluate the safety of an ocular wound chamber after a corneal injury in guinea pigs. The research group developed an ocular wound chamber that encases the eye and allows for controlled delivery of therapeutics and eye lubricant. Using OCT, intraocular pressure measurements, bright field and fluorescein imaging, and histology, they confirmed that the ocular wound chamber is safe for the skin and eye, and does not change wound healing when filled with optical lubricant.
The ocular wound chamber is a half-sphere—a cup—that attaches securely to the eye with a resealable port. Corneal injuries were caused by a corneal rust ring remover that stripped off the epithelium layer of the cornea. One group of guinea pigs were left untreated while another group received the ocular wound chamber filled with lubricant eye drops or lubricant eye gel. At 72 hours, no groups showed corneal fluorescein uptake, indicating they all achieved epithelial closure, though there was a trend toward slower closure with the lubricant liquid group. No statistically significant differences in intraocular pressure or histology was found among groups.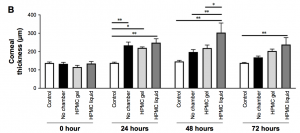
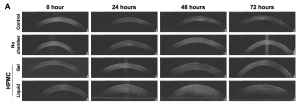
The Phoenix anterior chamber OCT took images of the guinea pig corneas (Figure 1) and the thicknesses were quantified in ImageJ. At 24 hours, all wounded eyes were significantly thicker than unwounded eyes (Figure 2). The untreated eyes returned to normal thickness 48 hours after wounding while the eye lubricant gel-treated eyes returned to normal 72 hours after wounding (Figure 2). The eye lubricant liquid-treated eyes were still thicker at 72 hours (Figure 2). McDaniels et al point out that it is thus important to consider treatment media of liquid vs gel when using the ocular wound chamber. Overall, McDaniels et al have developed a safe ocular wound chamber to protect and deliver treatments to injured eyes. Further studies will elucidate the effect of the ocular wound chamber in uninjured eyes and effects of using basic salt solution instead of eye lubricants in the chamber.